Universitetsavisen
Nørregade 10
1165 København K
Tlf: 35 32 28 98 (mon-thurs)
E-mail: uni-avis@adm.ku.dk
—
Science
Organoids — In body-temperature incubators at BRIC, a series of micro cancer tumours are growing — based on cells from real patients. The tumours can be used to test more than 1,000 alternative treatment options simultaneously.
In a laboratory at the Biotech Research and Innovation Centre (BRIC), four incubators have unusual contents.
The incubators are kept at a constant 37 degrees Celsius, because they contain tiny human cells that need to stay warm, grow, and develop — just as if they were still inside a real human body.
And even though the cells are nurtured and cared for with nutrient-rich protein gel, warmth, and careful handling, they are not particularly healthy. Quite the opposite.
How does the tumour develop? What alternative treatments might work for this specific patient?
Wojciech Senkowski, Assistant Professor, BRIC
The cells are, in fact, tiny cancer tumours formed from tissue samples taken from real patients with ovarian cancer.
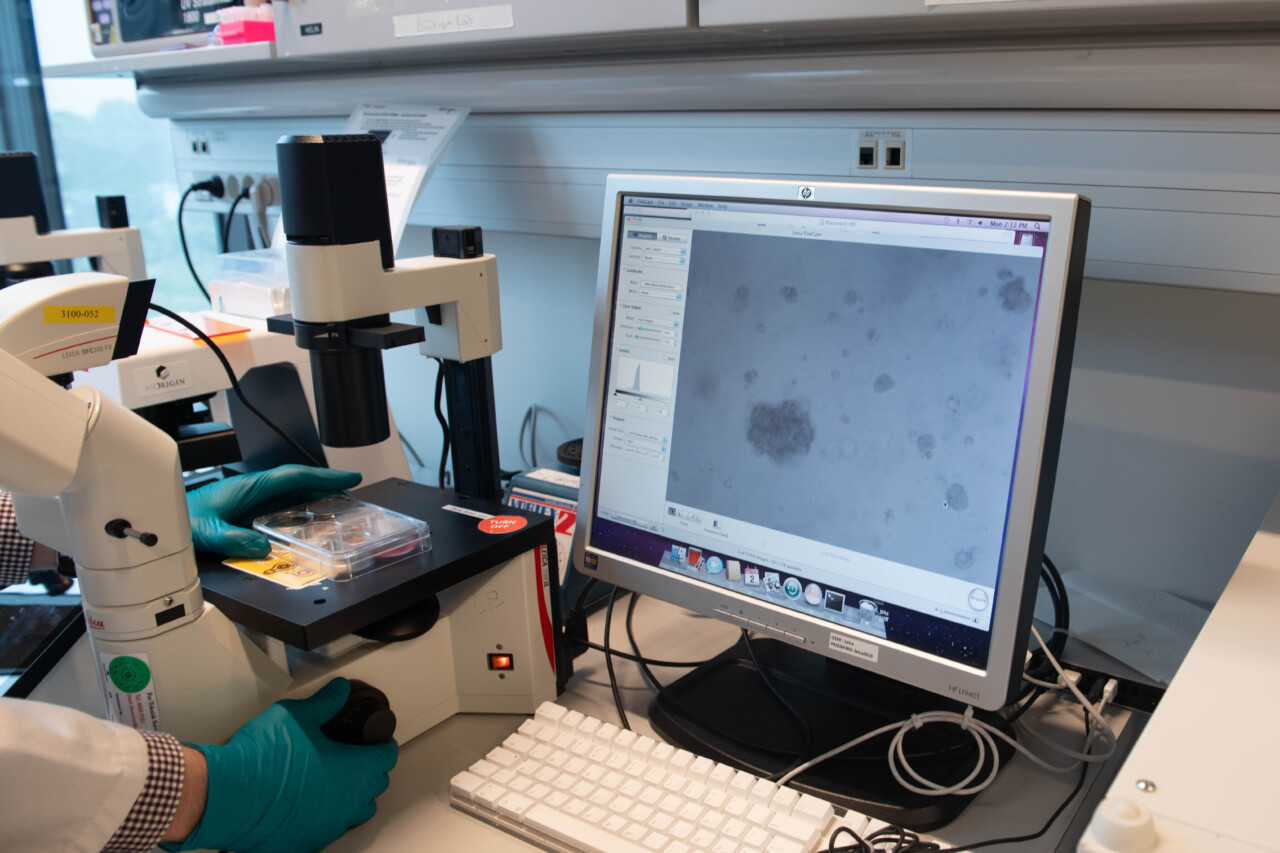
If you look closely at the coloured protein gel, you can see a series of bright spots that make up the cell mass. Place the mass under a microscope, and the cancer tumours themselves come into view:
Grey, misshapen objects embedded throughout the white mass, varying clearly in both shape and size from sample to sample.
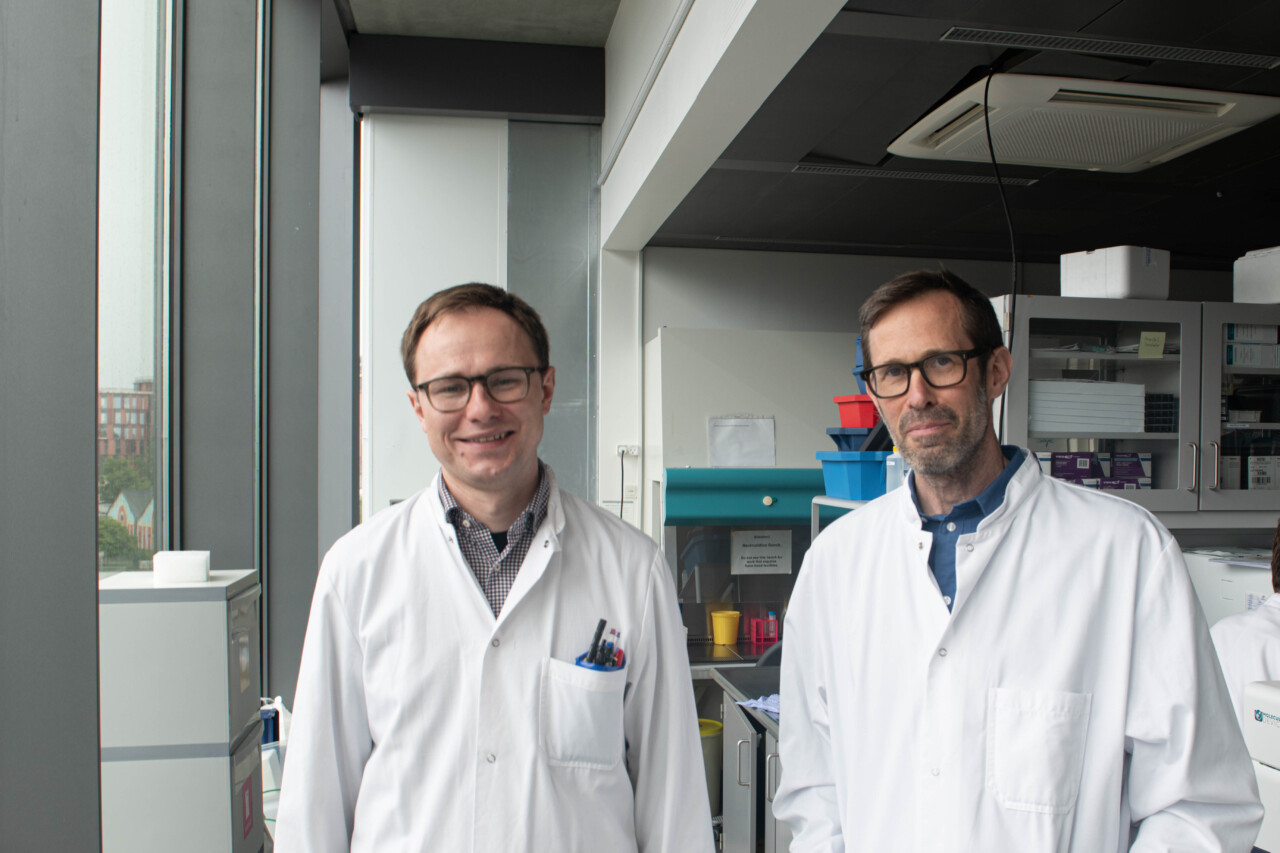
These lab-grown cancer tumours are called organoids, and according to the lead researchers — Professor Krister Wennerberg and Assistant Professor Wojciech Senkowski — they will offer deeper insights into ovarian cancer and be used for testing for a wide range of alternative treatments in the future.
The research project began as part of an EU initiative. It has been running for seven years and has since received funding from the Novo Nordisk Foundation, the Danish Cancer Society, Independent Research Fund Denmark, Innovation Fund Denmark, and the organisation OvaCure.
The core aim of the project is to explore how cancer treatment can be tailored to individual ovarian cancer patients, explains Krister Wennerberg.
»What is particular to ovarian cancer is that it often reemerges. We often see a patient treated with the standard methods — chemotherapy and surgery — and declared cancer-free. But after a few years, the cancer often returns — and then it’s difficult to treat,« he says.
Another defining characteristic of ovarian cancer is that it typically varies from patient to patient — which is why the research project focuses on exploring personalised treatment options.
»Every patient sample we receive is different — for example in the genomic composition of the cancer. That’s why we try to create our organoids as ultra-personalised models, where we preserve both the unique genetic profile, the structure, and the morphology of the original tumour,« says Wojciech Senkowski.
It took around two to three years to develop the first organoids, but once they figured it out, progress sped up. Today, there are 35 organoids in the BRIC lab — and the more organoids, the more answers, according to Wojciech Senkowski.
»Now we can begin to ask questions like: How does the tumour develop? What alternative treatments might work for this specific patient,« he says, adding:
»In some cases, we’ve even been lucky enough to get a sample from a patient when the cancer was first diagnosed and again if it came back. That’s incredibly valuable for research.«
To test alternative treatments, the tiny cancer tumour is divided into nearly 400 even smaller tumours, allowing the research team to test more than 1,000 different treatment options simultaneously.
»Then we see whether the cancer cells are destroyed or not. What works varies greatly from patient to patient. But recently we identified a potential new treatment that might work for around one quarter of all patients,« says Krister Wennerberg.
READ ALSO: When the cancer researcher’s husband got cancer
The research team discovered that some types of cancer cells were highly dependent on the so-called protein kinase CK2 to survive. Protein kinase CK2 is an enzyme that can be crucial for cellular processes, including signalling, cell growth, and death.
Ovarian cancer is the fifth most common cancer among women, and it is a very complex form of cancer
Wojciech Senkowski, Assistant Professor, BRIC
»We found that if we introduce medication that blocks the function of the protein kinase, the cancer cells have a harder time surviving. That’s why we believe some patients will benefit greatly from this treatment alongside standard chemotherapy,« says Krister Wennerberg, who adds that this would be relevant for about 25 per cent of patients with a particular genetic composition in their cancer.
The two researchers hope the discovery will lead to clinical trials, allowing people with this specific genetic profile and cancer type to try the treatment. And they are looking forward to this, because — as in much other research — the patients who donated cancer cells for the current organoids will not themselves benefit from the results of the research here and now.
»If you want to help the patient who donated the tumour tissue, you have to be quick. Often it takes months — maybe even years — before we receive the material, and by then the patient may no longer be alive,« says Wojciech Senkowski, and continues:
»As a donor, you are more likely helping the patients who come after you. And as researchers, we are very grateful to those who decide to contribute.«
Krister Wennerberg and Wojciech Senkowski were among the first in the world to develop ovarian cancer organoids. That is why they have also explored how to share both the models and the methods with the international research community.
»Legally and ethically, it is difficult to share the models, as they are based on cells from real people. But we collaborate with Finnish researchers in the EU project DECIDER, which collects samples from patients who have given consent for them to be shared,« says Krister Wennerberg, and continues:
READ ALSO: Overdiagnosis harms patients — professor calls for Danish medical education overhaul
»This means that it is possible to share many of the organoids with the research community via a biobank, Auria, which is located at the Turku University Hospital in Finland.«
Wojciech Senkowski adds:
»We also share our methods, so others don’t have to spend years trying to develop them.«
He explains that their vision is to one day create a virtual collection of different organoid models, accessible to researchers around the world. There are currently several research projects working with organoid models across various types of cancer.
»Ovarian cancer is the fifth most common cancer among women, and it is a very complex form of cancer. That makes the organoids difficult to create. We hope our work will make ovarian cancer organoids more accessible to researchers and help accelerate the discovery of new treatment options,« says Wojciech Senkowski.